By: Dr. Tanuj Palvia
What You Need to Know About Back Pain:
Everyone’s back pain is different.
Back pain is one of the most common health problems in the United States. It is estimated that 50 to 80 percent of adults have had back pain at some time and that 10 percent of all Americans have back pain in a given year. Back pain can occur at any age in both men and women and is one of the leading causes of disability and time lost from work.
Everyone’s back pain is different. While some conditions are hereditary, in many cases, your lifestyle contributes to your risk of back or neck pain. For example, if you lead a sedentary lifestyle or you’re overweight or obese, your chances of developing pain increase. Similarly, your risk increases with age as your muscles and connective tissue becomes less hydrated and more fragile.
Physicians typically aim to classify back pain into one of the three categories:
- Acute back pain – lasts from 1-7 days. Pain may be mild or severe and occasionally may be caused by an accident or injury. About 80% of all back pain is acute.
- Subacute back pain – usually lasts from 1-7 weeks and usually is mild; occasionally it’s severe. This pain generally is unrelated to other illnesses you may have. About 10-20% of all back pain is subacute.
- Chronic back pain usually lasts more than three months and may be mild or severe. It may be related to other illnesses you may have or may have no identifiable cause. About 5-10% of all back pain is chronic.
Let’s Talk About Anatomy:
The back is made up of the rear part of the body from the neck to the buttocks, with the main component being the spine. Like a modern skyscraper, the spine is a marvel of engineering that defies gravity, allowing humans to walk upright. It is strong and flexible, supporting the head and trunk of the body and enabling us to twist, turn, bend, and lift.
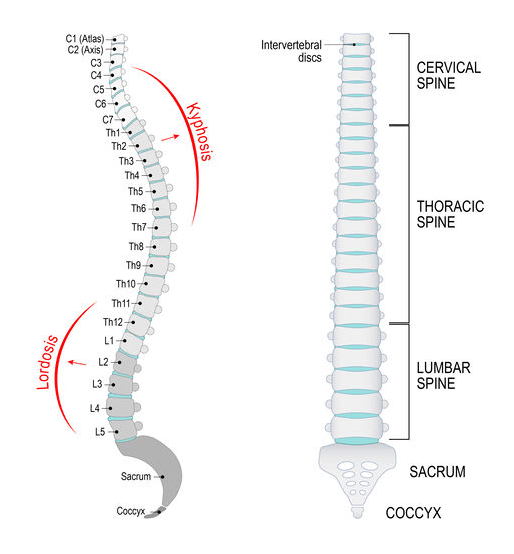
The spinal column is comprised of:
- 33 hollow, ring-shaped bones called vertebrae, which are separated and cushioned by 23 discs made of spongy cartilage.
- These vertebrae are divided into 4 sections:
- 7 vertebrae of the cervical spine in the neck
- 12 vertebrae of the thoracic spine in the chest
- 5 vertebrae of the lumbar spine in the lower back.
- The tailbone, comprised of the sacrum and coccyx
- The spinal column is supported and held together by a network of muscles, tendons, and ligaments.
- The spinal column forms a protective tunnel or canal for the spinal cord, the bundle of nerve fibers that transmit the impulses, or “signals,” to and from the brain that gives us the ability to feel and enable us to move. These are also responsible for conveying pain signals to the brain.
What causes back pain?
Before jumping into treatments for back pain, it’s critical to review what the targets for the therapy would be.
- Muscle strains and soft tissue injury: often caused by heavy lifting, turning, twisting, or sports-related injuries. This can often result in nagging spasms and trigger points.
- Bulging or herniated discs: discs are like cushions in between your vertebrae. These discs are filled with a soft material that can leak from a tear in the disc and press on a nerve in the spine. When this occurs it can cause tingling, numbness, and even moderate to severe pain.
- Osteoarthritis: causes a breakdown of the fibrous cartilage in the facet joints (joints that connect your vertebrae). Without the cushioning provided by the cartilage, your bones may rub together, causing pain.
- Degenerative Disc Disease (DDD): The discs cushioning the backbones begin to collapse – occurs when the discs in the spine begin to degenerate or weaken, causing pain, weakness, and numbness… Disc disease may be caused by genetics, obesity, or a minor injury that causes a herniated disk.
- Spinal Stenosis: occurs when your spinal column narrows and begins to put pressure on the spinal nerves.
- Loose ligaments around the Sacroiliac Joint: instability in the pelvis and may cause pain felt in the low back/hip area and may radiate to groin.
- Other causes: piriformis syndrome, coccydynia (tailbone pain), spinal fractures, non-musculoskeletal conditions including but not limited to endometriosis, cancer, abdominal organ disorders, infection, etc.
For a more in-depth conversation on what can cause back pain, watch these videos:
Back Pain, Part 1
Back Pain, Part 2
How to deal with back pain:
- Nutrition and healthy eating are powerful treatments to combat nutritional deficits that may be affecting your pain levels. Anti-inflammatory foods and a balanced diet of grains, vegetables, and lean protein help your body heal.
- Exercise can improve your pain by increasing flexibility and range of motion. Another benefit to exercise is the release of hormones called endorphins, your body’s natural pain relievers. You should consult with your doctor prior to exercising to ensure you are not causing additional damage to injured areas.
- Back braces may be all you need to get some support while you heal from an acute injury. Combined with proper nutrition and gentle exercise, back braces keep you active to help you regain your flexibility and range of motion.
- See an interventional pain physician. If the above fail, an interventional pain specialist can guide you through a short course of medication management to help facilitate a decrease of inflammation and relaxation of muscles. Sometimes an injection may help facilitate this in a more targeted and effective manner.
- Regenerative medicine is recommended for the continued strengthening and revitalization of deteriorated anatomy. Regenerative medicine will also increase functionality and longevity of these structures.
- Surgery is typically recommended when all conservative treatments are unsuccessful in reducing pain, recovering functionality, or if there is neurological compromise present, such as bladder or bowel incontinence, lower extremity weakness, spasticity, or loss of sensation. (I’ve shared my thoughts on surgery in this video.)
I generally recommend consultation with your physician if your back pain episode has not responded to conservative measures and/or has exceeded beyond 5-7 days. If you think we can help you, don’t hesitate to reach out to us by phone or by filling out the form below.