Mechanical traction therapy (or nonsurgical spinal decompression therapy) is a popular conservative treatment option for patients with low back and neck pain. Physio Logic Chiropractor, Dr. Mike Distler answers common questions regarding the treatment.
Is there a difference between traction therapy and decompression therapy?
The terms are used interchangeably, but traction and decompression are not descriptive terms for varying amounts of force. Decompression is the result of traction. It is inaccurate to suggest differing outcomes when comparing a device that claims to provide traction to one that claims to provide decompression. There may be a difference in patient comfort due to the design of the device, but current research demonstrates no difference in the ability of a specific brand of mechanical device to provide a better patient outcome when compared to other mechanical devices.
What is being decompressed?
Mechanical traction is performed on the low back or neck using a motorized system—typically with a harness—to provide decompression to the intervertebral discs of the lumbar or cervical spine. Traction can also be performed manually (i.e., without the assistance of a motorized device), but does not provide the same consistency in treatment force, duration, and positioning. Traction also has an impact on other tissues in the spinal region such as muscles and joints. Current research demonstrates that the stretch provided to these structures may contribute to the relief experienced from the procedure.
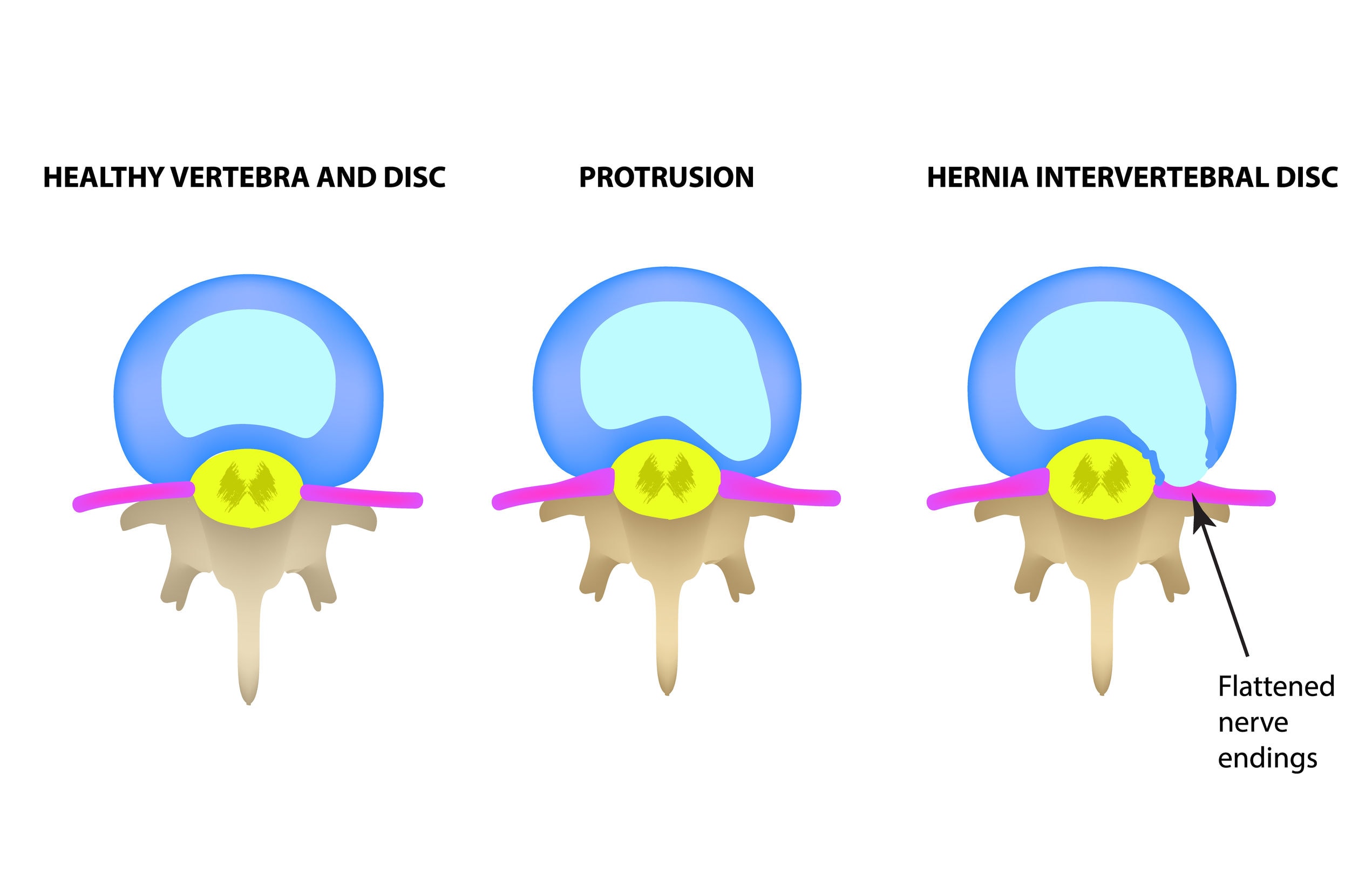
What happens to the disc?
In the simplest terms, traction unloads a compressed structure. During unloading, the axial stretch provided by the traction creates negative pressure inside the disc, which helps to provide relief by 1) facilitating the movement of nutrients into the disc and waste products out of the disc, 2) promoting retraction of a bulging or herniated disc that may be compressing other structures, such as a nerve. The purpose of the treatment is not to lengthen or “stretch out” the disc to a new height, but to improve the health of the disc through normal movements that have otherwise been compromised by injury. Research has demonstrated that intermittent traction helps to promote this process more than static traction.
How do I know if mechanical traction is indicated for my condition?
Traction is not indicated for all disc injuries. Even a bulging or herniated disc as diagnosed by MRI is not enough information to confirm that traction should be performed. As part of your initial examination, the provider will perform a series of tolerance and positional tests to determine if traction provides relief. Contraindications include spinal fracture, tumor, advanced osteoporosis, surgical hardware, and pregnancy. Current research suggests poorer patient outcomes for severely degenerated discs.
Is mechanical traction safe and how much do I have it be pulled?
Before treatment is performed, the provider will determine through examination whether mechanical traction or a different intervention is indicated. The therapy should be tolerable and should require the lowest force possible to provide relief, typically starting at 30-35% of total body weight for 15 minutes. The force does not need to be increased as long as the patient is experiencing relief; therefore, the ability to tolerate a stronger force is not a sign of progress. The force should be increased only if the patient no longer feels relief and traction is still an indicated treatment. An adverse reaction or no change in symptoms indicates that the treatment is not indicated under the current conditions.
How long does the relief last?
In the initial phase of care, relief should be felt immediately, but may return after 24 to 48 hours. As patients progress through the treatment plan, longer periods of relief are expected. Similar to any other form of musculoskeletal therapy, patient outcomes are improved when traction is performed as part of a multi-dimensional treatment approach. A recent study of cervical traction therapy concluded that a combination of mechanical traction and exercise therapy resulted in lower disability and pain over a 12-month period than exercise alone or a combination of exercise and over-the-door traction. Improvements in core stability, posture, ergonomics, and dysfunctional movement patterns can help change the stress being placed on the discs and improve long-term outcomes.
What is the difference between mechanical traction, inversion tables, and other forms of traction?
As discussed previously, the treatment should be performed at the smallest amount of force possible that provides relief. Motorized traction is the preferred method due to reproducibility in treatment force, duration, and position as well as better patient outcomes; however, subgroups of patients are able to achieve enough force via inversion tables or other forms of at-home traction (such as hanging from a pull-up bar) to provide decompression. If relief is provided with these non-motorized techniques, they should be performed systematically and with the same treatment protocol as motorized traction: intermittent traction for 15 minutes in a position that provides relief. If pain increases with any of these methods, stop treatment immediately.