You’ve probably discerned there’s SOME form of connection with the things you put in your mouth and your overall health by now. But have you thought about how the things you’re chewing on are affecting your mental health? In this article focusing on Nutritional Psychiatry, Physio Logic’s Clinical Nutritionist, Michelle Miller, MSACN; and Nutritional Educator & Registered Dietitian, Rachel Naar, RD, discuss how we ARE what we eat, and how in an era of mental un-wellness we can use nutrition to improve our mental health.
We Are What We Eat
The food we eat becomes the brain tissues, hormones, and building blocks of our cells that transfer information around our body which helps us do just about everything. We truly ARE what we eat.
Prebiotics work with probiotics, which are beneficial bacteria that live in our GI tract. Found in healthy, fiber rich foods like artichoke, garlic, and onion, prebiotics feed the probiotics to tame inflammation, and contribute to hormones that influence behavior. Probiotics also play a role in producing B vitamins, which help with tissue repair and energy metabolism.
Research has shown that certain dietary patterns are linked to changes in our brain that help the connections between our neurons.
Pretty cool, huh?
Introducing: Nutritional Psychiatry
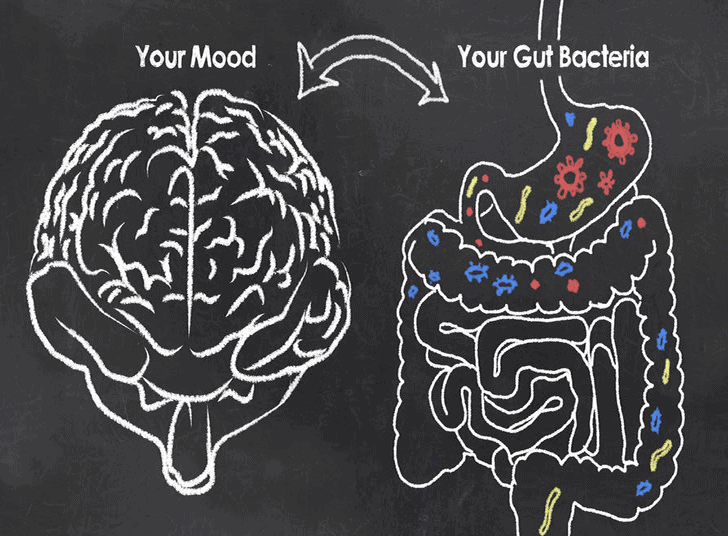
So if our brain cells are affected, our mood most likely will follow suit. Insert nutritional psychiatry, a new and exciting field exploring the connection between food and mood.
What is nutritional psychiatry and why is it relevant?
Nutritional Psychiatry is the theoretical framework of biological mechanisms whereby nutrition could exert its influence along a continuum ranging from general mental well-being to neuropsychiatric disorders.
- Nearly 1 in 4 Americans are diagnosed with some form of mental health issue each year
- The risk of depression increases by about 80% when you compare individuals consuming a diet high in saturated fat/trans fat/processed foods vs. whole-foods
- By 2020 depression will rank as the second leading cause of disability, after heart disease
Meet Our Second Brain
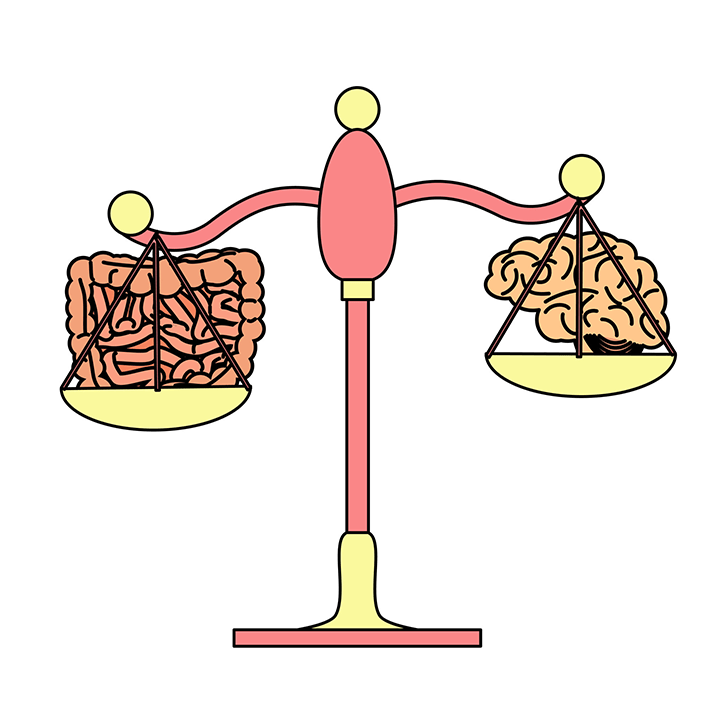
The Enteric Nervous System (ENS) consists of 100+ neurons that help our GI system function. These neurons line the esophagus, stomach, small intestine, and colon.
Think about it like a big game of telephone. It’s a network of neurons, support cells, proteins, and neurotransmitters, which are chemicals that send messages to cells.
Did you know the gut has more neurons than the brain, and that more than 90% of the body’s serotonin is in the gut?
Gut-Brain Connection
- An irritated GI can send signals to the brain that trigger mood changes and vice-versa
- GI distress can be the cause or the product of anxiety, stress, or depression
- Irritable Bowel Syndrome (IBS)
- Nausea felt before a presentation
- GI distress/diarrhea during a panic attack
- Irritable Bowel Syndrome (IBS)
- GI distress can be the cause or the product of anxiety, stress, or depression
Gut Dysbiosis
One of the tell-tale signs of poor mental health is not necessarily cognitive, but may originate in your gut!
If you can’t move your food through your body, you end up with dysbiosis (which is an imbalance of the good bacteria in your gut).
As a result you may develop yeast infections, enzyme deficiencies, and small intestinal bacterial overgrowth (SIBO), as well as a slew of food intolerances.
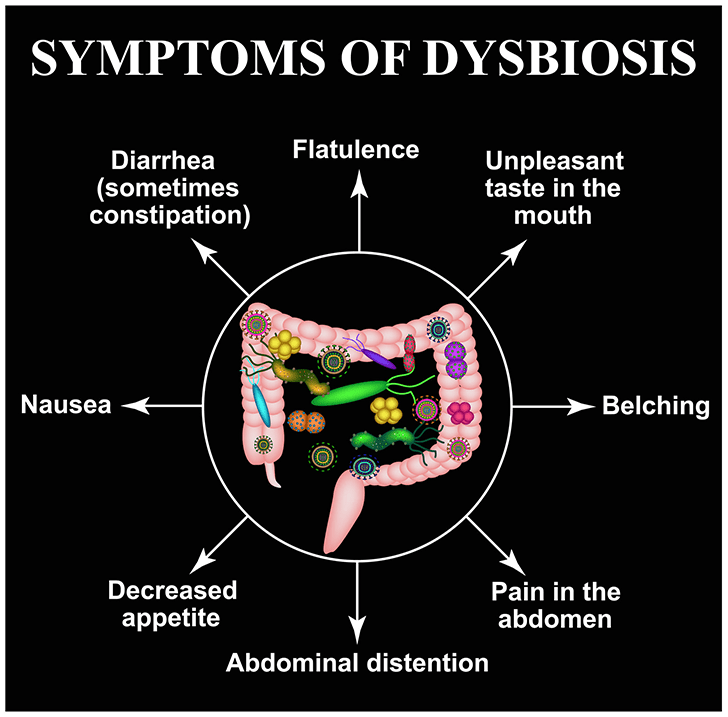
Prolonged GI distress can lead to depression, anxiety, and other mood-related disorders as a result of an imbalance of these microbiota and hormones.
This begs the question; if you can heal your gut, can you heal your brain?
The Research
The ‘SMILES’ trial was a randomized controlled trial aimed to investigate the efficacy of dietary improvement for the treatment of major depressive episodes. The study looked at utilizing nutritional counseling sessions focused on a Mediterranean diet (EVOO, fish, nuts) vs. solely social support sessions.
The dietary intervention group demonstrated statistically significant improvement on depressive symptoms vs. the social support group.
Omega 3’s, Please
- Alpha-linolenic acid is an Omega 3 fatty acid that is essential in the diet because it cannot be synthesized by humans. Ex. walnuts, flaxseed
- Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are very long chain Omega-3 fatty acids that are contained in fish and shellfish (omega-3 FA)
Research suggests that greater intake of Omega 3’s are associated with reduced risk for developing mood symptoms.
- Habitual fish intake is correlated with greater Omega 3 levels
- US has 2-fold lower seafood consumption vs. Japan
- Shifts away from fish-based to Western diets were associated with increased rates of seasonal affective disorder, depression, Coronary Artery Disease, suicide
Putting it all together
- Sending Love to your GI
- Microbiome and byproducts play a role in brain function and behavior
- Prebiotics we eat to feed the microbiome and can change the nature of bacteria resulting in mood fluctuations
- Eating in a way that promotes good gut health includes adequate fiber intake from fruits and vegetables
- Stabilizing your Blood Sugar
- Blood sugar changes can accentuate psychiatric conditions and associated behavioral disturbances
- Protein and healthy fats can contribute to stabilization of blood sugar levels with emotional improvements
- Dietary Guidelines recommend limiting added sugars to no more than 10% of your daily intake
- No more than 6-9 tsp (25-28g)/day
- Coke has 39g of added sugar in a 12oz bottle!
- No more than 6-9 tsp (25-28g)/day
| Nutritional Factor | Implication | Foods |
| Pyridoxine (Vitamin B6) | Produces serotonin, a neurotransmitter that regulates mood/sleep | Spinach, Salmon |
| DHA (Omega 3) | Major building block of the brain, produces hormones that protect neurons | Tuna, Algae |
| Prebiotics | Provide fuel to our microbiome | Garlic, Onions |
Follow Rachel for more nutrition news at @naartrition
References:
- Polyunsaturated fatty acids and recurrent mood disorders: Phenomenology, mechanisms, and clinical application.
- A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial).
- A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults.
- Moving towards a population health approach to the primary prevention of common mental disorders
- Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis.