Low Back Pain management with Regenerative Chiropractic Solutions
By: Dr. Stephen Szaro, DC, and Dr. Tanuj Palvia, MD.
Low back pain is the leading cause of disability globally. It is estimated that 80% of Americans will experience back pain at some point in their lifetime and the prevalence of low back pain is on the rise. Also, 7 in 10 people with back pain will have a new episode each year. A small percentage of people (about 7%) will develop chronic or disabling pain.
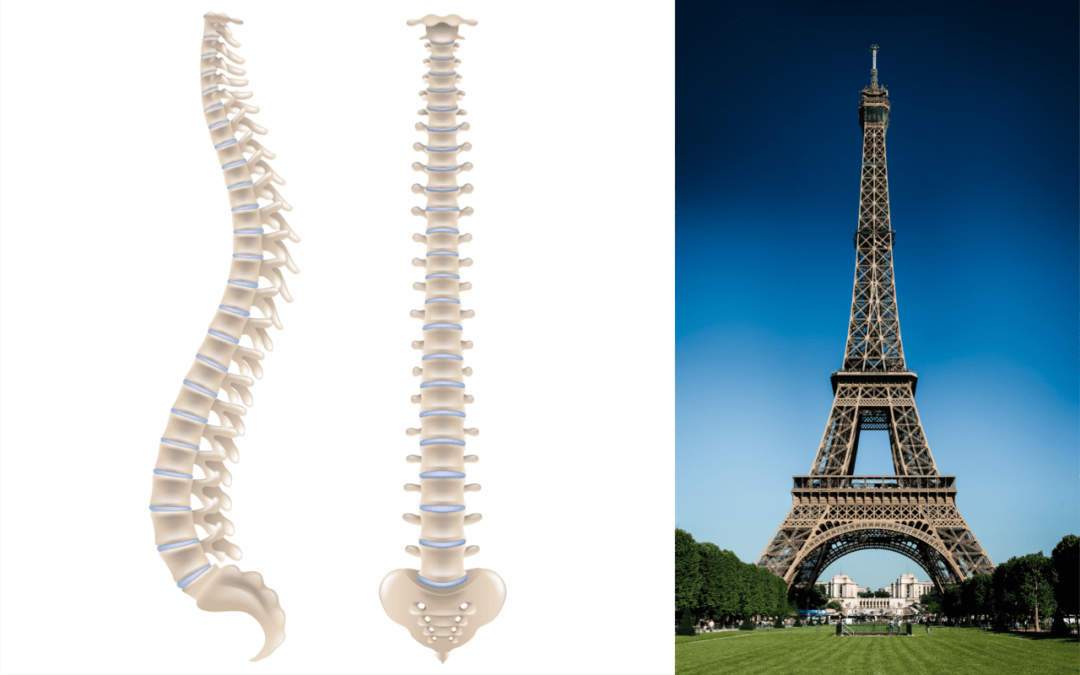
The symptoms and severity of low back disorders vary depending on the cause. Symptoms can include local pain, pain that refers to or travels into the pelvis, hip(s), down the legs, or up the back to even the neck! The back is a complicated structure of bones, joints, ligaments, and muscles, that work together to form a complex yet dynamic scaffold that supports your entire body.
Why Low Back Pain Occurs
You can sprain ligaments, strain muscles, herniate or rupture disks, fracture a bone, or irritate joints, all of which can lead to back pain. While sports injuries or accidents can cause back pain, sometimes the simplest of movements or repetitive movements—for example, picking up a pencil from the floor— can have painful results. In addition, arthritis, poor posture, obesity, and psychological stress can cause or complicate back pain. Back pain can also directly result from disease of the internal organs, including but not limited to kidney stones, kidney infections, pancreatic disease, blood clots, or bone loss.
When discussing the causes of low back pain with your provider, it is important to discuss the most common medical diagnoses that are known to cause back pain based on the anatomy. However, we now understand that the structure does not always dictate whether or not a patient will experience pain. For example, the evidence clearly shows that there are many people who have herniated discs in their lower back and may never experience pain or have limited pain throughout their lives. Therefore, it is extremely important to discuss the relationship between symptomatology with respect to pain and function/movement issues when establishing a proper diagnosis and treatment program.
- Facet Joint Pain – Pain originating from inflammation or degenerative changes of the joints that connect the vertebrae of the spine. The facet joints are necessary for allowing motion of the spine through several planes. If there is inflammation of degenerative changes present it can severely limit motion or cause significant pain.
- Herniated or Bulging Discs – Often referred to as a slipped or compressed disc. Your discs act as the shock-absorbing structures of your spine. Think of the discs like jelly donuts. The jelly (nucleus) on the inside absorbs the compressive loads the spine deals with on a daily basis. The outer layer (annulus) is very strong and made of collagen fibers that protect the nucleus. If the annulus becomes damaged the nucleus can escape or herniate and can cause irritation or direct pressure to delicate spinal nerves. This can lead to what many patients describe as a pinched nerve or “sciatica”.
- Osteoarthritis/Degenerative Joint Disease/ Degenerative Disc Disease – These are terms used to describe degeneration to the discs and facet joints of the spine. The discs can become desiccated and compressed and the bones and joints can form bone spurs or osteophytes. This degeneration leads to worsening inflammation and altered and poor spinal movement which will cause pain.
- Sacroiliac Joint Pain – Pain originating from inflammation to the joints that connect the sacrum or tailbone to the pelvic bones. This is more common in females especially pre and post-partum due to the release of hormones that cause ligaments around the joints to become lax.
- Spinal Stenosis – Stenosis refers to compression of the spinal cord or its surrounding tissues due to disc herniation or osteoarthritic changes usually causing a specific set of symptoms.
- Spondylolisthesis – This occurs when one spinal bone (vertebrae) has “slipped” forward or backward on the bone above or below it. This is usually caused by a degenerative phenomenon but can also be caused by an acute injury.
- Sprains/Strains – Sprains occur when there is an injury to the outer layer of the discs or the ligaments that support and protect the spine. Strains occur when there is injury, overstretching, or spasms of the muscles that assist in the movement of the spine. These conditions can occur from an acute injury such as a car accident or lifting something heavy or can occur from cumulative or repetitive injury over time.
- Spinal instability – Instability refers to the inability of the muscles to protect the spine from excessive motion during the spinal movement. The muscles of the “core” need to protect the spine by making it rigid while we move. For example, when we lift a suitcase off of the floor, the muscles of the core will stiffen to protect the spine and discs before we lift the heavy load. If the core is not working properly it leads to instability of the spine and an increased likelihood of injury.
Chiropractic Intervention
The main goal of the chiropractic exam is to determine the root cause of the injury or condition. If, during the exam, it is determined that the patient is showing significant signs of inflammation, muscle spasm or there is a significant amount of spinal degeneration it is imperative that the patient be co-managed with an interventional pain medicine specialist as we will discuss later. Without co-management, it may be difficult to improve functionality when high levels of inflammation are not brought under control.
Next, and for the simplicity of this article, the chiropractor should determine whether or not the patient fits into one of two categories. Does the patient have a condition related to a structural problem, such as osteoarthritis or disc herniation, or do they demonstrate a movement disorder, such as poor spinal motion due to lack of spinal/core stability? In reality, most patients who have structural spinal problems also have a movement disorder, however, not all patients who have movement disorders have structural spinal problems.
- Spinal Manipulation – Manipulation or chiropractic adjustments are important to restore proper spinal motion to joints that have lost their ability to move through the full range of motion. Joints typically become less mobile due to acute or repetitive injury and is a protective mechanism used by the body to avoid further injury. Manipulation is extremely effective to restore motion to immobile joints and can significantly reduce pain.
- Myofascial Release – Sports massage techniques such as Active Release Technique and instrument-assisted soft tissue massage techniques aid in reducing muscle tension/spasm, fascial restrictions, and scar tissue. This will improve mobility, reduce pain, and assist the patient in performing the corrective and rehabilitative exercise.
- Rehabilitative Exercise – Initially, exercises should be performed to reduce pain and improve mobility. Once the patient is out of acute pain it is imperative to load the spine properly and challenge the core musculature and gluteal complex in order to improve the resiliency of the spine. This will help patients develop improved spinal stabilization with regular daily activities and will help avoid injury with simple movements such as bending and lifting.
- Spinal Decompression Therapy – When patients are diagnosed with conditions such as disc herniation or spinal stenosis, decompression therapy can be extremely useful in many cases. The goal of decompression therapy is to relieve compression on injured discs, joints, and nerves and allow healing to take place. With the proper diagnosis, patient positioning, and traction parameters spinal decompression therapy can help many people with chronic spinal pain and reduce the need for surgery.
Interventional Pain Medicine
As is the common theme of this blog series, pain can limit the recovery of functionality and can stall your rehabilitation program. Therefore, concomitantly with rehabilitation, an interventional pain physician can oftentimes perform minimally invasive outpatient procedures to help enhance and expedite the decrease of inflammation that may be limiting your recovery.
When you see an Interventional Pain specialist, a thorough history, physical exam, and diagnostic tests (e.g., x-rays, CT scan, MRI, and possibly blood tests) are used to evaluate your situation and identify the exact pain generating tissue that is preventing your recovery. At this time, it might be determined that a minimally invasive interventional treatment is advisable to address this injury. For back pain, some of these modalities are listed below, with explanation:
- Trigger Point Injection: the use of anesthetic to break muscle spasms that are unresponsive the manual manipulation
- Epidural Injection (in all areas of the spine): the use of anesthetic and possibly steroid medications injected into the epidural space to relieve pain or diagnose a specific condition, such as lumbar radiculopathy or spinal stenosis.
- Nerve, Root, and Medial Branch Blocks: injections done around nerves to determine if that specific spinal nerve root or nerve branch is the source of pain. Blocks also can be used to reduce inflammation and pain.
- Facet Joint Injections: an injection used to determine if the facet joints of the spine are the source of pain. These injections can also provide pain relief. This typically is useful in arthritic pain that comes from these joints.
- Discography: an “inside” look into the discs to determine if they are the source of a patient’s pain. This procedure involves the use of a dye that is injected into a disc and then examined using an x-ray or CT Scan.
- Radiofrequency Ablation: a minimally invasive procedure that disables spinal nerves and prevents them from transmitting pain signals to the brain.
- Spinal Cord Stimulation: the use of electrical impulses that are used to block the pain from being perceived in the brain.
- Percutaneous Discectomy/Nucleoplasty: a procedure in which tissue is removed from the disc in order to decompress and relieve pressure.
- Sacro-iliac Joint Injection: the use of anesthetic and possibly steroid medication injected into this often pain-producing joint between the spine and pelvis to relieve inflammation and facilitate recovery.
- Regenerative Medicine: a combination of platelet-rich plasma and/or stem cell therapy can be used to fortify any weak ligaments/musculature that has developed due to chronic injury, or to heal discs or facets (joints) that have been damaged due to disc disease, arthritis, or trauma.
Working together, an interventional pain management specialist and a chiropractor can design a comprehensive pain program specifically for you as you recover, which may include a combination of ongoing interventional treatments and the continuation of rehabilitative services. All of these services are offered at Physio Logic, eliminating the need to go from place to place to receive care.
If you’re experiencing low back pain and want to know you’re getting every available option to recovery, give us a call or start by filling out the form below.