Michelle Miller and Diana Orchant host the hit Functional Medicine podcast, FUNC YOU UP! You can listen to it on Google Podcasts, Apple Podcasts, Spotify, or wherever you get your podcasts. This article is a transcript of Episode 48, IBS is BS. Enjoy!
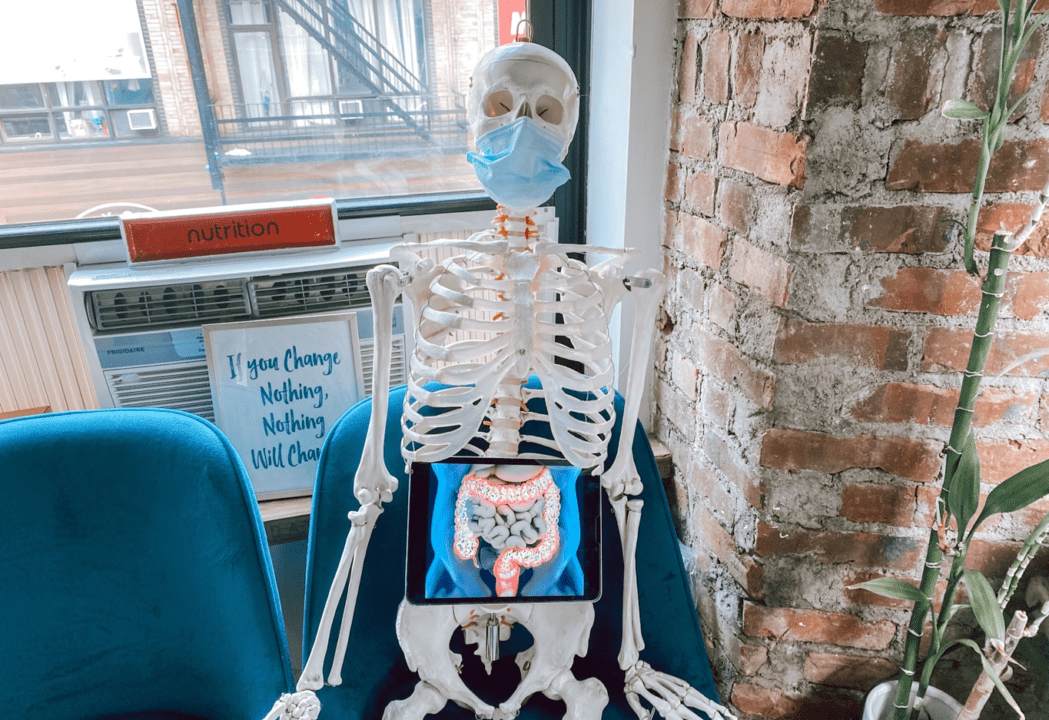
IBS, or Irritable Bowel Syndrome (IBS) is the most common gut disorder. What frustrates us about IBS? There’s a lot of things, but the number one reason is it’s a diagnosis based on exclusion. IBS is an umbrella term used when they don’t know what’s actually wrong with you.
In other words, after ruling out several other possible causes, they diagnose you with IBS. Individuals with IBS can experience a wide variety of symptoms. When we really start to break them down, it gets to a point where it seems like who doesn’t have IBS? Which can be scary.
IBS Symptoms
When looking at the commonly suggested symptoms of IBS, it’s things like:
- Abdominal Pain
- Acid Reflux
- Nausea
- Bloating
- Constipation
- Diarrhea
There are three types of IBS based on your symptoms. There’s IBS-D for diarrhea, IBS-C for constipation, and IBS-M for mixed diarrhea and constipation. These are really just signs from your GI system indicating something isn’t right, but now we’ve put a label on it.
So, did that really fix anything? Did you really need to know that you’re this label of your bowels being irritable? I think you already knew that if you were having all of these symptoms.
Medications for IBS
Dozens of medications can be used to help with these symptoms. You’ve probably seen them walking down the aisle of your local Duane Reade or *****
For example, there’s the Pepto-Bismol jingle (“Nausea, heartburn, indigestion, upset stomach, diarrhea – Yeah, Pepto Bismol!”) that everybody knows. That doesn’t actually heal your body. You’re not deficient in the ingredients of Pepto-Bismol, that’s just a band-aid effect. Covering up the symptoms.
There are stories of patients who are using products like MiraLAX every day as a part of their supplement regimens to deal with their constipation. That’s not a long-term game plan. That’s really just covering up a symptom that your body is trying to loudly tell you some things that are off.
We need to move away from managing symptoms and taking these medications every day to make sure you can go to the bathroom, to actually getting to the underlying cause.
Why aren’t you going to the bathroom? Why are you going far too often? Why are you running to the bathroom three times before you have a big interview?
What is Good Digestion?
It’s important to break down what good digestion should look like.
Good digestion is not where you have tums in all of your coat pockets, in bags, because you just know that you could get reflux at any time.
Let’s start with upper digestion. Then we’ll work our way down.
Good Upper Digestion
Good upper digestion is where there really isn’t anything happening. You’re not really noticing any signs of nausea, or belching, or hiccups.
You’re not having:
- Indigestion
- Acid reflux
- Bloating
- Stomach aches
- Stomach pains
- Cramping
You don’t get the feeling that food is kind of just sitting. It’s not getting digested, this idea of being distended or having frequent flatulence. None of this should be happening.
You should ultimately be unaware of digestion happening as long as you’re eating an appropriate amount.
Then, in terms of bowel movements, this is always something that really surprises my clients. We speak about this with such ease because we literally talk about this all day long. It’s like the weather.
At Physio Logic, I’ll have to say normal and healthy terms of bowel movements is one to three bowel movements a day. That’s regular, consistent, predictable so that you’re not seeing a lot of variation in the consistency, the size, the frequency.
Everyone does get their own “normal” within those parameters.
Some people will say, “my normal is to go like twice a week.” So, I guess the difference between normal and common is probably what we should be talking about. It really isn’t that healthy. Healthy is going one to three times a day and fit to be a healthy consistency, not running to the bathroom.
Things like bloating after lunch are something that we hear all the time and it’s not normal. We want to just get across that no one should have to live this way. At the same time, instead of normalizing some of these things, we want to make people aware that these are warning signs.
You don’t just have IBS for life – things manifest. This is a kind of inflammation that starts in your gut and works its way around the body. To quote Hippocrates, “disease begins in the gut”. So, if we sent you home with one thing, it’s that absolutely, yes.
Let’s start with creating this paradigm shift of not symptom treating. We’re not trying to manage the diagnosis of this disease. We’re really trying to get to the underlying root cause of it.
So for us, that always starts with running the proper tests and doing the proper assessments upfront so that we really know what we’re working with and we’re not doing trial and error with patients.
Running Tests
The first testing that we do at Physio Logic in NYC, is the comprehensive stool test analysis. This three-day stool test gives us a lot of information. Anything from asking if your body is secreting enough enzymes to break down food?
Do you have any types of bacteria issues? Either not enough good bacteria, some bad bacteria, yeast, or candida, fungal strands. Basically, any imbalance in the gut flora, also referred to as dysbiosis.
It’s either not enough good stuff or too much bad stuff. Then things like parasites, which nobody wants to see included. It’s not fun to deliver that news, but a super common symptom that obviously goes misdiagnosed.
Often clients will come to us and mention completing a stool test with their doctor. The thing is if you compare the comprehensive stool tests that we have you do, versus the stool tests that you might do with your standard gastroenterologist, nothing wrong with either of them, just the gastroenterologist is usually not testing for a lot of these fungal strands and the things that Michelle said was enzyme activity.
They’re more looking for the pathology of the disease. Like, let’s use this as a test for further testing. Do we need a colonoscopy? Do we need an endoscopy? Does this person have stamina, like things that are alarming and need to be treated with medication usually right away?
It’s that high-level stuff. That’s kind of the newer role of conventional medicine. That high level, more acute emergency care, which is great.
Testing with a GI Doctor
When we find out a client’s had a colonoscopy or endoscopy, or that they’ve done this testing with their GI doctor because that does ensure that a lot of the more serious stuff has been ruled out and that we have so much more to work with now that we don’t have to worry about that stuff.
Just like a blood test, when a doctor orders a blood test, they’re choosing what they’re checking off. What markers to order to see anything with a stool test. So there are tons of parasites, so there are strands that you’d have to be looking for if your doctor is not checking off to be checking all of those things, that’s why it’s not coming back. It doesn’t mean that it was not present. It just means it wasn’t looked for.
I think that’s a big point of distinction that is not often made or talked about. So sometimes individuals might have more upper or even middle kinds of GI symptoms. Whether that be belching, nausea, or poor digestion.
We’ll often need to look for small intestinal bacteria growth overgrowth, which we have a whole separate episode just on CBO for you. CBO stands for small intestinal bacterial overgrowth. So, these breath tests really test for different hydrogen and methane levels in our GI system.
So, sometimes they’re actually often about 15% of people with IBS often have CBO that has not been diagnosed. This bacteria is being released by the gas and is being released by the bacteria.
That’s moved it’s way up into the small intestine where it shouldn’t be. Honestly, it’s a resilient bacteria. It’s a tricky thing to treat and to address. I think one of the great things about our integrated team at Physio Logic is we kind of all approach it from a different standpoint and you can clear that good bacteria out and really rebuild the gut.
Sometimes that’s the entire IBS issue for some clients. Sometimes it’s just a piece of the puzzle. Not everybody with IBS will have it, but it’s certainly something that can’t go without checking. You know, checking out and looking into.
The other testing that we always do is blood work. So blood work surprisingly can actually tell us a lot about various IBS cases, right? We’ll look at cortisol, which is your main stress hormone.
Inflammation Tests
So if you’re really stressed, a lot of time, people with IBS are running to the bathroom before a stressful situation. We can look at inflammatory markers with a test for inflammation, ultimately dying in the entire body. As well as food allergies, food sensitivities, which actually pick up quite a bit.
I was doing a live webinar on IBS and we got into a really good conversation. Some of the questions about the impact that hormones have on IBS.
The idea came up about a woman who is getting her period who could have constipation a few days before her period. Then she starts to have diarrhea during her period. We’ve had these patients and they’re like, I only have GI issues for a week and a half or two weeks around my cycle.
That’s half of every month, which is why we’ve got to get to the root of that problem. So yes, it’s healing the GI system.
Balancing Hormones
Well, you can’t forget about the other kind of secondary issues, which could be balancing hormones. There are a lot of things that we’ll see on the blood work. So, now let’s just dive into our approach for getting to the root cause of the patient coming into Physio Logic, kind of what types of things that we would do to mitigate IBS and really figure out what’s actually going on.
So let’s start out with functional medicine and functional nutrition. There’s kind of a widely used gut protocol. You might hear it referred to as the forearm protocol or a five or six-hour protocol where we’re expanding at some times. It’s basically the idea of late, like removing all of the triggers.
So this could be parasites, bacteria, yeast. It could be inflammatory foods and removing anything that’s causing inflammation.
kind of getting that out of the system. I think that this is like pulling the weeds in the garden, just clearing all that stuff out, and then it’s replaced with good things. This could be prebiotics, this could be enzymes. If those levels are low, these could be anti-inflammatory foods. This could be anti-inflammatory herbs, healing the gut, which could be things like bone broth or collagen or marshmallow root…
Then replacing or reinoculating, we think of that as like adding all the good bacteria back into the gut so that yes, we’ve removed all these bad things, but we want to make sure we have that good gut flora flourishing.
Restoring the Gut
This is like receding the population, receiving the garden, putting those good probiotics in there, maybe using some free Biotics to make sure that they have some fuel. Working with the diets, make sure you have a good enough fiber in the diet and the right types of fiber and the diets are feeding all of that too.
So we don’t have the exact same approach with every single patient on what enzyme you’re using, let alone like what healing agent we’re going to use to repair. I think that’s like more of a personalized tactic that you look at the energy of the herbs, the energy of the person, and kind of what their underlying needs are, but that’s a general idea of how this process of healing the gut goes.
I think what a lot of people miss out on is really this idea of what else is happening outside of just the four R program or the five R program things. Like the liver being sluggish or really getting to the root problem of food sensitivities.
So I think, at Physio Logic, we have this hybrid approach to both and do an elimination diet. An elimination diet is where we get rid of the main food triggers, main food allergens, foods that people generally tend to react to without even knowing it.
Our Hybrid Approach
So this hybrid approach is kind of the 10-day elimination detox, where we throw in some herbs to really support the liver, the three phases of detoxification and also get rid of this gluten, soy, corn dairy, just to name a few of the main food allergens it will get rid of. Of course, alcohol as well.
Just to figure out and kind of calm all the inflammation and then slowly add back all the various foods after we’ve detoxified to see how our body then reacts. That’s often a way that we identify food sensitivities, there’s also more extensive testing, but that can usually be, like, one of the most effective ways to just figure it out right there.
So, this idea of liver detoxification can get a little tricky to understand. Isn’t that like the whole idea is that the liver is supposed to be detoxing all day long, 24 seven?
A really great analogy for this that I use with patients. I used it earlier today with a patient. So break down a dishwasher analogy. So we’ve talked about this and you’ve heard us on previous podcasts about this topic, but essentially our liver is supposed to be detoxing.
That’s what its job is. Our liver’s main job, right? To get rid of these toxins in the body that are not supposed to be there. However, the same way we go through a spring cleaning, you want to kind of detoxify, give that liver a little bit of extra boost.
So, we have this dishwasher analogy. That’s super easy to understand where a restaurant has a normal influx of clients coming in eating dinner and they’re sending their dishes to the back. In the back, the dishes are being cleaned. It’s a nice little cycle, but let’s say that it’s a holiday and everybody’s rushing into the restaurant and you have so many people way more, you have extra staff.
However, the dishwasher is still this unit that’s one size. So you start to throw in more and more and more dishes and the dishwasher gets backed up. So you have to slow things down and kind of take a step back and help that dishwasher.
Every, let’s say twice a year, for example, that’s a good analogy for how our liver also needs that extra help ever so often. That’s what this detox and elimination diet really does for your body. I mean, we live in a toxic society. There are a lot of things that can bog down and cause this like, quote-unquote, sluggish liver, and the idea of medications having to be processed.
Liver Processing
Our foods have to be processed through the liver. Obviously things like alcohol, but especially processed foods, corn syrup, a lot of these like trans fats, that stuff is harsh to digest. I mean, that is not easy on the liver. Just as much as alcohol is.
Then of course we said medications also, if there are things in the body like heavy metals or I think even things we don’t even think about, like an oral contraceptive pill or Advil that we’re taking. Not a common basis, high levels of product.
Especially now with COVID, we’re all using more Clorox and Lysol and all these products that we’re really not supposed to be using that frequently, let alone, we’re not wearing gloves when we’re using it, wiping down tables.
It’s getting into our skin and getting into our system and all those chemicals. There are also just things that we see on blood work, like high cholesterol that’s a burden to your liver. Just a good reminder that we do this with the seasons as well, that there’s often at least once, if not twice a year, it is good just to kind of give a little spring cleaning for your body to a little oil change and just make sure that everything is functioning at optimal capacity.
Our Liver Detox System
So, going back to this idea, hearing this process, it’s like a liver detox with an elimination program. I’ve seen a lot of different types in this field, ranging anywhere from 30 days, or maybe even as short as 14 days, all the way to 120 days.
They can be really grueling and it’s usually a really strict, structured diet. So it’s kind of saying goodbye to your life for a little while because you have to just stay on such a regimented program in order for it to really work and for you to really identify these potential symptoms of food sensitivities.
The idea that we kind of figured out, we can hack this by hearing the detox with the elimination diet, because when you go through this process of removing all these inflammatory foods while supporting this liver detoxification and all of those pathways, you get all these other levels to start dropping these histamine levels, other inflammatory levels.
So it’s just a little bit more of an efficient way to kind of go about it. Then after the 10 days, you start testing these foods back out when maybe every other day, or every third day.
I think what we have found with our clients is they just have a little bit more of an obvious response. At the end of the day, maybe it only took two and a half weeks to figure all of this out. So it’s not a perfect system and we do have to change it up for some people and kind of personalize it a bit more for some individuals than others.
I wish more people would do this. Because I think it would take away the bad name, elimination diets have kind of helped to move things along a little bit more. The next thing we usually test is blood chemistry, as I mentioned a little bit earlier. We’ll start to look into things that then also can bog down the liver such as hormones, right?
GI Distress
If your hormones are imbalanced, it can also lead to high levels of estrogen. Let’s talk about GI distress.
It’s not uncommon that we see women with estrogen dominance. This just means, you have far too much estrogen that your liver is not able to filter through. For example, a little bit more testosterone, that can cause a lot of GI issues as well.
So sometimes addressing those underlying hormones that we’re testing through your blood can really tell us a lot about what’s going on in the body. Also nutrient deficiencies, right? I’m thinking vitamin D, various B vitamins.
B vitamins are super important for our energy, vitamin D for the immune system. If we’re kind of low in a lot of these various vitamins and minerals, it can cause a lot of inflammation.
What else do we test in the blood? I mean, looking at the good, healthy levels of cholesterol to see if healthy fat levels are there. It’s interesting because it’s kind of this double-edged sword of potentially you’re not getting enough nutrients because you’re not able to absorb them well enough because of something going on with this underlying cause.
Do you have low enzymes? You can absorb your nutrients or is there so much inflammation in the gut from so many sense sources or triggers that the micro VLI. In the intestine trying to collect all the nutrients isn’t as effective as it used to be. Also having these nutrient deficiencies causes a lot of the secondary symptoms of IBS, like anxiety, depression, and fatigue, brain fog. So it gets really tricky.
Why Blood Work is Important
I think that’s why we take the blood work just as seriously as a lot of the other tests, because we know we need to replete those nutrients ASAP so that we can just get somebody feeling better and maybe just getting their energy up little bit. So they feel like they can tackle something like a 10-day elimination diet.
What’s interesting is saying that we were down these micro VLI, that’s really what happens when we have a lot of inflammation. Resulting in a leaky gut. Let’s back it up a minute. Let’s go back to the microbial. Just, so everybody understands, we’ve all heard this term, or maybe we haven’t, but it’s very common, this whole kind of term of leaky gut. And what that really means is our gut flora.
Leaky Gut Syndrome
They have these little microvilli. You have, like, these long fingers that are really great for absorbing all the nutrients, right? So when your food starts going through the stomach, the GI system, these microbes are absorbing all these nutrients.
However, let’s say that there’s a virus that comes through, whether it be food-borne pathogens, like salmonella or something, that’s a little less obvious, such as undiagnosed gluten sensitivity, right?
So something that you are not aware of, whether it be gluten or maybe a food allergy or a sensitivity to dairy. Let’s say there’s all these different factors, right. But over time that starts to create inflammation in the body.
What that looks like in terms of your GI system, is these little microbes start to wear down. So all you have left are really, like, if you make your hands into fists are all kind of these fists. So you don’t have these fingers, these microbes alive that are able to absorb all these nutrients.
So over time, the tight junctions of the gut, or I guess these microvilli that are kind of all intertwined start to separate, and that’s how you start reacting, right? So even though you’re eating so much broccoli and kale and good quality quinoa and things like that, your body is looking at them all as these foreign invaders, because your gut starts to be so inflamed. These tight junctions start to become looser junctions and so little pieces of broccoli and chemicals on the good foods, readings start to get into the blood, which raises every systems antenna saying, let’s become inflamed. That’s essentially leaky gut.
I remember doing like a lab practical on this, where we had a sifter and it was like, we pour water through it and then pour sand in and then put like gravel, and it was like, okay, well obviously the gravel doesn’t go through.
Some of the sand goes through and like the water goes through, but we think of those as the nutrients that are going into the bloodstream, those are the things that are supposed to pass and like the rocks and the pebbles and the gravel can pass through. Then basically we messed with the sifter and made it so that more stuff could pass through. That was like the inflammation damage that would take place.
Leaky Gut and Healing
Now suddenly little pieces of shale and gravel were passing through, that ends up in the bloodstream where it’s not supposed to be in your body’s very, very well versed on what’s supposed to be there and what’s not supposed to be there.
It sets off an alarm and it tags that. It says, anytime I see that we go to up-regulate our immune system and inflammatory pathway and go after those guys. What if that’s like a chicken protein, or what if that’s lettuce or something that is technically a good food, but now you’ve tagged it as a bad food.
This is often what I’ll see when clients come in and they’ll say, I feel like every year I’m restricted like my body can’t handle more and more food. I feel like the list of foods that I can’t tolerate is rolling, People come in with a list of 25 foods they can’t tolerate.
That is like leaky gut all day long. So yes, there could be a lot of other things going on, but if you don’t ever heal, you can do the program until the cows come home until you do a leaky gut, make sure that you’re removing the contributing factors to inflammation.
You’re really allowing that lining to heal and seal. Your inflammatory pathway is what’s going to lead everything. So that once we get you back up and running, you’re less likely for this to occur.
IBS and the Diet
We’re nutritionists, so we have to discuss diet and lifestyle. So we kind of touched on this here and there, but really through all of this various testing, we always have to address vitamin and mineral deficiencies.
This usually comes in at the last of the strategy of reinoculating, right? Because we’re throwing in good bacteria, whether it be probiotics prebiotics to help grow those probiotics, but then also different micronutrients that now that we’ve healed that leaky gut, we can start absorbing again, also during this phase, this is when we’re going to look a little bit deeper into.
Some of the foods that are long-term, you just might not have an easier time to deal with, even if they’re not food sensitivities.
This may be when we’ll have conversations about some of the high FODMAP foods or, some foods that have higher fructose content. Sometimes that can be an issue with IBS patients. The idea is to really allow you to consume as great of a variety as possible while avoiding anti-inflammatory foods and avoiding ongoing damage and symptoms day-to-day.
Now, this is going to vary greatly from one individual to another. We usually try to find certain, we don’t subscribe to any one diet. I think we really kind of find a range of diets between elements of the paleo diet, or elements of the keto diet.
We like elements of the Bulletproof diet or elements of the whole 30 diet. I think we kind of pull from a lot of those when we’re talking to a patient, seeing what their favorite foods are culturally, what foods they’re drawn to, and really trying to design a game plan around that long term.
IBS and Lifestyle
I also think a lot of the lifestyle elements tend to be kind of overlooked. It can’t be understated how important those are.
So talking to Diana, she’ll take us through some of the ones that she really thinks make the biggest impact with our IBS clients.
So I’d say the first one is really sleeping. I think we overlook sleep as such an important. Getting at least seven to eight hours, if not more, sometimes your body needs more, especially while it’s repairing and healing.
Getting those 7-8 hours a night and really having good quality sleep, no animals jumping in the bed, not being awakened ever. Some of it is sometimes out of our control, but doing what we can because those sleeping those hours at night are so important to repair and heal and detoxify our body to toxify so much at night.
Which is why we would say wake up in the morning and have some water because your body’s been working really hard all night. Gotta give it a little bit of water. Then the other one I would say is really important and I know there’s so much laughing.
Whether that be watching a funny TV show, YouTube video, just sitting with your partner, or your friend and video chatting or hanging out and just getting that true, like deep belly laughs. So, it is important just to kind of relax and enjoy life a little bit.
It’s to not be super uptight. So you’re it. I love that you pointed that out specifically because there are so many benefits that happen.
So if you’re laughing, you’re automatically out of the fight or flight response, you’re automatically out of that, like cortisol driven stress response, you’re getting more oxygen to your body because you’re breathing in a different way when you’re laughing, you’re having feel-good endorphins and neurotransmitters circulating because it’s an enjoyable experience.
I think it’s just as good, like mentally as it is physically for that. I think also the same idea with a gratitude practice, typically you’re grateful for those moments of laughing and being happy and joyful.
Movement and Exercise
So it kind of goes hand in hand with that. I also think just proper movement and exercise, depending on the severity of a GI case, we have to be careful with how much exercise or movement is sometimes that can actually put too much stress on the system.
Getting outside, safe, healthy movement is essential for our body. Good circulation again is itself kind of neat oxygen going to all the cells of the body, putting the GI system. So we need everything kind of moving and circulating.
I think often stress is a component that can be frustrating for IBS patients because a doctor or practitioner will say, you need us, you need a stress reduction practice. You need to reduce stress. You need to be less stressed.
I think let’s stop pretending that just talking about it is going to do something you have to really put in the work.
It’s just as hard as changing your diet. So really committing to a movement practice and really committing to a stress reduction or a mental, I consider it like a mental health practice.
So, this idea of meditating is great, or doing yoga, or going on a walk, in nature. All of those things are fine. It could be doing breathwork. It could be singing. It could be like doing a dance class. It could be really anything you want it to be as long as it’s reducing stress and bringing you joy.
It’s all just kind of revolving around this idea of getting you out of the fight or flight response, getting you breathing, bringing some joy to your life, getting those feel-good hormones going.
IBS and Mental Health
I think we’re in a stressful time right now. I think there’s a lot of worry. It’s so important, especially because a lot of IBS is all mental.
Figuring out what works for you, whether it be learning how to take a deep breath. Sometimes we think we’re all stuck in shallow breathing. Whether it be just sitting outside in the sun, like figuring out what works for you just to keep you calm and kind of static throughout the day, instead of having these high highs, low lows, and moving up and down in our stomach, just going with it.
I also think this is probably if whatever the hardest thing for you to do is probably the area where you should call in help. We’re hired because people need help with creating a plan to get their health and their diet back on track.
Get Help at Physio Logic
So if you’re finding that your finances are stressing you out, hire a coach. If you’re finding that you aren’t committing to your workout regimen, hire a coach. If you’re finding that, you’re not meditating, get a group of people together and create an accountability situation.
I started doing breathwork classes because that wasn’t something I was going to do on my own. I was not making it a priority. So I needed to put some skin in the game and kind of like suck up the ante and step up my commitment to it.
I also think that’s an important thing to do as well as just know yourself. If it’s something you want to do, there are ways that you can get it done. You might just need to call in and some experts, so you can really make sure that happens. Everyone’s experience with IBS, as with any symptoms and situations, is really going to be different.
So Michelle and I have really laid out, I think kind of like an extensive high over kind of what IBS can be, what the various triggers are, what a lot of the underlying causes are.
There’s really no one-size-fits-all for really anything in functional medicine.
But as it pertains to IBS right now, there’s really no kind of band-aid approach one size fits for everyone. So we’re here just to kind of lay it out for you and give you all the various options and the different paths that we would go down if you came in as a patient. Michelle Miller and I, Diana Orchant, are available to discuss you individual concerns via virtual consultation so, if you think we can help, give us a call or start by filling out the form below.